Stereotactic radiation therapy is a treatment option for tumors that are hard to reach or cannot be removed surgically, with less damage to normal tissues and fewer treatment days needed compared to traditional radiation therapy.
Key Takeaways
- Stereotactic radiation therapy is very effective, and causes fewer side effects than conventional radiation.
- How long it takes for stereotactic radiation therapy to work depends on the exact cancer type and how quickly it divides. Rapidly growing cancers typically respond quickly, while slower cancers will respond more slowly.
- SRS cancer treatment for dogs means stereotactic radiosurgery. This is very similar to stereotactic radiation therapy (SRT), but is only done in one treatment.
- Side effects of stereotactic radiation for dogs include skin irritation, tissue death, and rarely organ failure.
When Veterinarians Recommend Stereotactic Radiation Therapy for Dogs
If available in your area, your veterinarian or veterinary oncologist may recommend stereotactic radiation therapy for dogs with tumors that cannot be removed surgically or are hard to reach.
It may also be recommended for tumors near or part of vital organs (ex: heart base tumors, brain tumors, etc.).2 Stereotactic radiation is more precise than conventional radiation, making it less likely to damage these delicate and important tissues.
You can also opt for stereotactic radiation even if your dog could benefit from conventional radiation. The smaller number of treatments and lower risk of side effects are very attractive for many dog lovers.
How Stereotactic Radiation Therapy Works
In general, radiation therapy involves sending ionizing radiation into a tumor to cause damage to the DNA and other molecules in the cancer cells.1 It will also damage non-cancerous cells in the field of radiation.
Traditional fractionated radiotherapy uses a high total dose of radiotherapy that is split up into many smaller doses, typically over 3-4 weeks.
Stereotactic radiation therapy (SRT) uses an overall smaller dose of radiation, however it is given in fewer visits with higher doses given per visit.
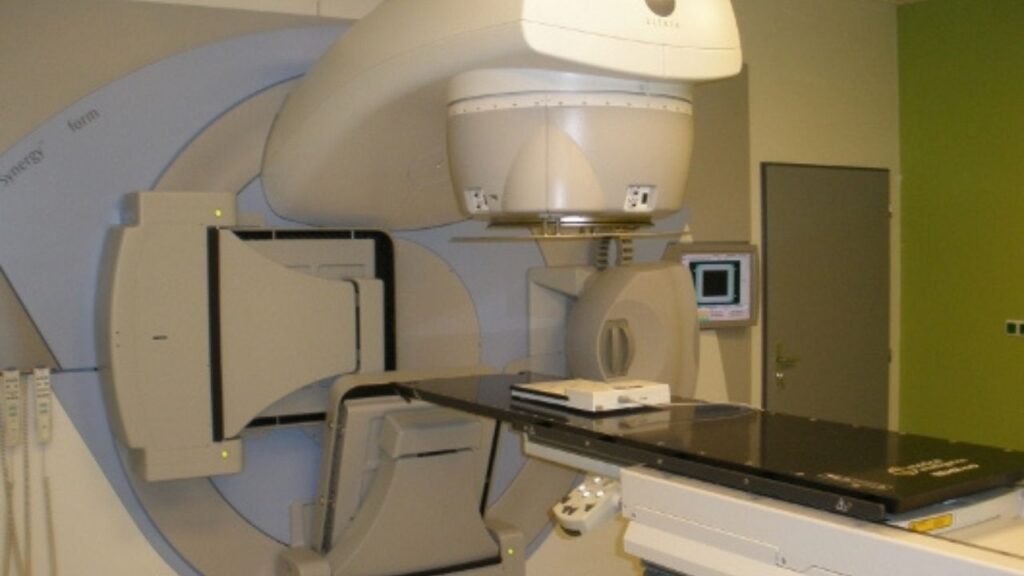
SRT is also different because it uses advanced imaging and robotics to precisely line up the radiation equipment to ensure that the radiation is delivered to a highly specific area, thus saving as much non-cancerous tissue as possible.5
Cancers SRT Is Commonly Used For
- Brain tumors1,2,6
- Bone tumors including osteosarcomas (this is typically just for pain control/palliative care)7
- Nasal tumors1,2,8
- Multilobular osteochondrosarcoma1,9
- Pituitary tumors1,3
- Thyroid tumors1,10
- Heart base tumors1,11
- Mast cell tumors12
- Soft tissue sarcomas13
- Tumors in the pelvic canal1,2
Common Examples of SRT
Prescriptions for radiation therapy are written as the number of fractions (doses) of the amount of radiation given.
Radiation is measured in Gray (aka Gy). For example, five doses of 4 Gray would be written as 5Gy x 4 Fractions.
- Example: Pituitary tumors: 15 Gy x 1 fraction or 8 Gy x 3 fractions3
- Example: Nasal tumors: 9-10Gy x 3 Fr4
The most important thing for you to know is the number of fractions your dog will receive, as this is the number of days you need to bring her in. But if you’re interested, the oncologist can walk you through your dog’s total planned radiation dose and the dose for each fraction.
Radiation specialist Jenny Fisher takes us behind the scenes for a tour of radiation. Great DOG CANCER ANSWERS episode!
What Happens During Stereotactic Radiation Treatments
Before treatments are given, your oncologist will want to get a complete and detailed image of your dog’s tumor.
- Your dog will be taken into the hospital for advanced imaging (typically a CT scan) under anesthesia to image the tumor completely.
- The radiation oncologist takes the imaging of the tumor and creates a stereotactic radiation plan using specialized software.
Once the radiation oncologist has a plan, they will schedule your dog’s treatments.
- Most SRS plans consist of 1-5 treatments within one week.
- Your dog will undergo anesthesia (usually light anesthesia) while the radiation is delivered.
During the treatments, specialized equipment sends beams of radiation to the tumor from different positions. The software used to plan treatments determines how to aim the beams so that the maximum amount of radiation hits the tumor, and minimal radiation hits normal tissue.
Once the procedure is over, your dog wakes up from anesthesia. Once they have recovered from the anesthesia, they either go home for the evening or stay in the hospital for the night.1,2
How to Get the Best Results
Since the procedure is performed under anesthesia, it is best not to feed your dog on the morning of SRT.
After radiation therapy, your dog’s skin may be irritated in the radiation area, so avoid exposing the skin to excessive sunlight or applying creams or lotions, which can cause more irritation.
There is mixed evidence about the use of antioxidants with radiation therapy. Theoretically, antioxidants (vitamins A, C, and E, silymarin, etc.) help repair cells from radiation-induced damage. However, they may also help cancer cells repair themselves. In general, most radiation oncologists recommend refraining from taking supplemental doses of antioxidants during radiation therapy.14,15,16
Home Care
After your dog has completed their radiation treatments, you will likely be sent home with pain medications and/or anti-inflammatory drugs to help with side effects.
You mustn’t apply any ointments or creams to the skin that may be inflamed without consulting your radiation oncologist first. It’s counterintuitive, but many ointments and creams can worsen radiation side effects.
Many general practice veterinarians are not familiar with post-radiation care, so make sure you discuss this with the radiation oncologist, and follow their advice.
Most dogs just need pain medication, time, and an e-collar (cone) to prevent scratching. Some dogs will also benefit from soft food if the radiation therapy is performed near their mouth.17
Follow Up
Recheck appointments will be recommended to you by the radiation oncologist based on your pet’s specific condition and treatments. However, imaging is typically repeated every six months afterward (or as recommended) to monitor for regrowth.
Rechecks may also be needed to manage side effects.1
When to Not Use Stereotactic Radiation for Dogs
Stereotactic radiation cannot be used if no visible tumor is present on imaging. For example, tumors that have been removed but without clean margins are not candidates for stereotactic radiation.
It is also not typically used for metastasized tumors (spread to other body parts) unless used alongside chemotherapy.1 While the SRT will target the primary tumor, the metastases will not be within the radiation beam.
Caution should be taken with SRT for heart base tumors. If they are slow-growing and not causing problems for the dog, SRT may not be the best approach since it may cause life-threatening arrhythmias.11
Acute and late side effects can be worsened if radiation therapy is used in conjunction with some other cancer treatments including doxorubicin, dactinomycin, fluorouracil, methotrexate, bleomycin, nitrosoureas, and etoposide.18 If your dog is receiving any of these drugs, radiation therapy may not be appropriate.
Where to Get Stereotactic Radiation
Stereotactic radiation therapy is available only at specialty veterinary hospitals with radiation oncologists. The equipment to perform this type of radiation is extremely expensive and requires a lot of safety measures to protect staff, so many facilities do not offer this treatment.
To find a hospital that can perform radiation therapy, visit vetcancersociety.org/pet-owners/find-a-vcs-member/.
Some of these locations may not offer SRT specifically.
Side Effects
Side effects depend on the area of the body undergoing radiation therapy. With stereotactic radiation therapy, there should be fewer side effects than conventional fractionated radiation therapy. However, side effects are still seen.
These can be divided into acute (short-term) and delayed/late (long-term) side effects.2
Acute Side Effects
These typically occur at the time of radiation therapy or shortly after. Examples of acute side effects include erythema (redness of the skin), oral mucositis (ulceration of the oral cavity), and arrhythmias (if treatment is for heart base tumors).
Short-term side effects are usually “self-limiting,” meaning they resolve independently with pain management and supportive care. They also typically affect only rapidly dividing tissues (skin, intestinal lining, oral mucosa, etc.).
Delayed or Late Side Effects
These occur months to years after treatment and are less common (fewer than 5%), but often more severe and difficult to treat.
Examples include fibrosis (scarring), necrosis (tissue death), organ failure, fistula formation, strictures, and cancer. These delayed or late side effects tend to damage slow-growing tissues in the bone, lungs, heart, kidneys, and nervous system in the path of radiation beams.
These serious side effects occur in less than 5% of patients, usually during the five years after treatment occurs.
Costs
The cost will depend on the hospital, but estimates are around $6,000-10,000 depending on the specific treatment.
Additional follow-up imaging (CT scans) range between $1500-3000 depending on location, and additional hospitalization or treatment costs may be present if there are side effects.
- LaRue, S. M., & Gordon, I. K. (2013). Radiation Therapy. In 2181272856 1500149962 S. J. Withrow (Author), Withrow & Macewen’s Small Animal Clinical Oncology (5th ed., pp. 180-197). Elsevier.
- Bloomfield R. Stereotactic radiation therapy in veterinary medicine. Can Vet J. 2015 Jan;56(1):95-7. PMID: 25565724; PMCID: PMC4266068.
- Hansen KS, Zwingenberger AL, Théon AP, Kent MS. Long-term survival with stereotactic radiotherapy for imaging-diagnosed pituitary tumors in dogs. Vet Radiol Ultrasound. 2019;60(2):219-232. doi:10.1111/vru.12708
- Custis JT, Harmon JF, Ryan SD, et al: Canine nasal tumors: A stereotactic radiation therapy approach. Presented at the ACVIM, Denver, June 16, 2011.
- Rancilio, N. (2021, October 06). Conventional versus stereotactic radiotherapy. Retrieved November 16, 2022, from https://todaysveterinarypractice.com/oncology/conventional-versus-stereotactic-radiotherapy/
- Griffin LR, Nolan MW, Selmic LE, Randall E, Custis J, LaRue S. Stereotactic radiation therapy for treatment of canine intracranial meningiomas. Vet Comp Oncol. 2016 Dec;14(4):e158-e170. doi: 10.1111/vco.12129. Epub 2014 Dec 18. PMID: 25524449.
- Martin, TW, Griffin, L, Custis, J, et al. Outcome and prognosis for canine appendicular osteosarcoma treated with stereotactic body radiation therapy in 123 dogs. Vet Comp Oncol. 2021; 19: 284– 294. https://doi.org/10.1111/vco.12674
- Mayer, M. N., DeWalt, J. O., Sidhu, N., Mauldin, G. N., & Waldner, C. L. (2019). Outcomes and adverse effects associated with stereotactic body radiation therapy in dogs with nasal tumors: 28 cases (2011–2016), Journal of the American Veterinary Medical Association, 254(5), 602-612. Retrieved Nov 16, 2022, from https://avmajournals.avma.org/view/journals/javma/254/5/javma.254.5.602.xml
- Sweet KA, Nolan MW, Yoshikawa H, Gieger TL. Stereotactic radiation therapy for canine multilobular osteochondrosarcoma: Eight cases. Vet Comp Oncol. 2020 Mar;18(1):76-83. doi: 10.1111/vco.12481. Epub 2019 Jun 17. PMID: 30989784.
- Lee BI, LaRue SM, Seguin B, et al. Safety and efficacy of stereotactic body radiation therapy (SBRT) for the treatment of canine thyroid carcinoma. Vet Comp Oncol. 2020;18(4):843-853. doi:10.1111/vco.12625
- Magestro LM, Gieger TL, Nolan MW. Stereotactic body radiation therapy for heart-base tumors in six dogs. J Vet Cardiol. 2018;20(3):186-197. doi:10.1016/j.jvc.2018.04.001
- Lurie D. Clinical case study: Radiation therapy for facial mast cell tumor in a beagle. https://www.dvm360.com/view/clinical-case-study-radiation-therapy-for-facial-mast-cell-tumor-in-a-beagle. Published May 24, 2021. Accessed November 16, 2022.
- Gagnon J, Mayer MN, Belosowsky T, Mauldin GN, Waldner CL. Stereotactic body radiation therapy for treatment of soft tissue sarcomas in 35 dogs. J Am Vet Med Assoc. 2020;256(1):102-110. doi:10.2460/javma.256.1.102
- Moss RW. Do antioxidants interfere with radiation therapy for cancer?. Integr Cancer Ther. 2007;6(3):281-292. doi:10.1177/1534735407305655
- Simone CB 2nd, Simone NL, Simone V, Simone CB. Antioxidants and other nutrients do not interfere with chemotherapy or radiation therapy and can increase kill and increase survival, part 1. Altern Ther Health Med. 2007;13(1):22-28.
- Borek C. Antioxidants and Radiation Therapy. The Journal of Nutrition. 2004;134(11):3207S3209S. doi:10.1093/jn/134.11.3207s
- Radiation therapy – side effects. Veterinary Specialty Center. (2022, November 3). Retrieved November 16, 2022, from https://www.vetspecialty.com/specialties/medical-and-radiation-oncology/radiation-therapy-side-effects/
- Cox JD, Ang KK, Moss WT. In: Radiation Oncology: Rationale, Technique, Results. 9th ed. Philadelphia: Mosby Elsevier; 2010.
Topics
Did You Find This Helpful? Share It with Your Pack!
Use the buttons to share what you learned on social media, download a PDF, print this out, or email it to your veterinarian.