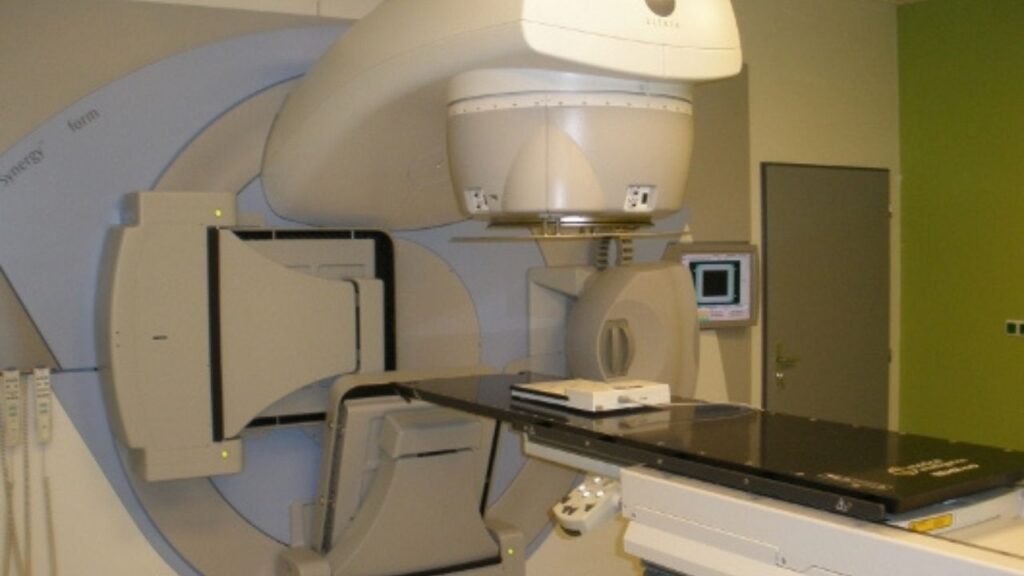
The CyberKnife® is an image-guided robotic machine that provides concentrated, pain-free, high-doses of radiation to tumors with marked precision. Cyberknife for dogs is expensive and only available in a few places, but it may be worth the trip if your dog’s tumor is hard to access.
Key Takeaways
- CyberKnife is typically used for cancers that can’t be treated safely with traditional radiation or surgery. There is some evidence to suggest that in brain cancers in dogs, CyberKnife is more effective overall than conventional radiation.
- CyberKnife is non-invasive and painless. It’s also expensive. If your dog has an inoperable tumor that cannot be treated, particularly if it is causing pain (as most tumors in the head do), it is worth considering if it’s in your budget or covered by insurance.
- In 2014 the cost of imaging, treatment, and anesthesia for treatment with a CyberKnife was between $7,500 to $8,000.
- Cyberknife is typically used to treat brain tumors, nasal tumors, and less commonly, bone cancers. It is also sometimes used as a follow-up treatment for complex or difficult surgeries, or less commonly for palliative pain relief.
- CyberKnife shrinks tumors (decreases their size or stops them from growing), by depositing high doses of radiation with precision in tumors. The radiation damages the DNA in cancer cells so they start to die off. Depending upon where the cancer cell is in its reproductive cycle, it may die right away or within a few months.
About CyberKnife®
The CyberKnife® system was developed in 1989 by Dr. John Adler as a method to treat tumor masses in humans using stereotactic radiation therapy (SRT).3 Since then, CyberKnife has become a radiation treatment option for canine companions as well.
Radiation with the CyberKnife is non-invasive, painless, and can be highly individualized to your dog’s specific treatment needs. It can be used to treat cancerous as well as non-cancerous tumors throughout the body in a much shorter time period than can be achieved with conventional radiation methods.
CyberKnife is particularly useful for targeting tumors that are inaccessible, complex, or otherwise not candidates for surgery.
What Happens When Using CyberKnife to Treat Cancer
CyberKnife is a image-guided robotic machine that provides high doses of radiation to extremely precise locations.
The overall goal is to provide a high dose of radiation to damage the DNA in cancer cells. DNA that is damaged has a more difficult time replicating, greatly reducing the tumor’s growth rate. Damaged DNA can also cause cancer cells to undergo apoptosis (death), thus decreasing the size of the tumor as well.
CyberKnife is very precise, and very potent. There is a lot of planning done before actual treatment. Here’s what you and your oncologist can expect.
Imaging
Advanced imaging is needed to determine the specific areas to be targeted. This is typically achieved with computed tomography (CT scan). A CT scan informs the veterinary oncologist where the cancer is in your dog’s body, as well as the size and shape of the tumor(s).
Your dog may also receive or need magnetic resonance imaging (MRI). MRI is better at detecting certain types of cancer. If your dog’s tumor is in the head, MRI will almost certainly be used.
Plotting the Treatment Field
Next, your radiation oncologist will feed these images into a software system. That sophisticated software constructs a 3D plan for the radiation treatment of your dog.
The software essentially plots coordinates for the CyberKnife, providing a map of where radiation should be administered with millimeter to sub-millimeter accuracy.
Treatment Sessions Are Planned
Radiation using the CyberKnife is typically an outpatient procedure, meaning your dog typically does not need to stay at the hospital overnight.
Treatment depends upon the type and size of the tumor being treated and can last anywhere from 20 minutes to 3 hours.
This doesn’t mean your dog is in one treatment for all that time. Instead, CyberKnife is performed over the course of multiple sessions, also called fractions. The number of fractions will be different depending upon the type and size of the tumor. Still, there are considerably fewer treatment sessions in CyberKnife than when conventional radiation is used.
Day of Treatment
One of the great benefits of the CyberKnife is that the machine is intuitive and can readily respond to changes in body position from breathing, coughing, moving one’s head, and tensing muscles. This is wonderful for safety reasons. However, dogs still require anesthesia during treatments, just to make sure they stay as still as possible.
Once under anesthesia, your dog will be put into the proper position. This position is dictated by the software’s plan. The radiation staff will use various equipment to keep your dog in the right place, including a formed cushion, moldable thermoplastic shells, and/or a skull fixation device.
Once your dog’s personal 3D plan is programmed into the machine, the CyberKnife will then move and bend around your dog, providing a calculated high concentration of radiation on the tumor while minimizing radiation (irradiation) to healthy tissue.

Is CyberKnife Surgery?
You may hear the CyberKnife referred to as a method to perform radiosurgery. This is misleading. The procedure is noninvasive and does not involve any cutting of tissue. The term “radiosurgery” simply refers to the fact that the radiation performed by the CyberKnife is able to accomplish what surgery could accomplish if it were an option.
Even though your dog will be put under anesthesia, the procedure done with the CyberKnife is not surgery. CyberKnife is truly a type of radiation therapy.
When CyberKnife Is Recommended
So, when might veterinarians recommend the CyberKnife over surgery or conventional radiation treatments?
- Typically, the CyberKnife is used when a tumor cannot be reached using surgical means. Tumors may be too complicated for surgery, or in areas of the body that are inoperable.
- CyberKnife may also be prescribed as a follow-up treatment after difficult surgeries to further ensure that remaining cancer cells are destroyed.
- The CyberKnife may also be recommended for dogs with tumors located in regions of the body that can be removed, but whose owners do not wish to amputate. For example, a dog with a history of back problems might not be a good candidate for amputation.
- Dogs who have tumors that have not responded to other methods, such as conventional radiation, may be candidates for the CyberKnife, with the hope that it will be more successful than previously failed treatment types.
- While less common, the CyberKnife may also be recommended as a method of providing palliative therapy. Dogs with large tumors can receive some relief with the CyberKnife as it helps to shrink the tumor, even when it is not likely that the tumor will be fully eradicated.
What Makes CyberKnife Special
The precision of the CyberKnife allows it to deliver higher doses of radiation than can be achieved with conventional radiation. This means it’s more effective at damaging the DNA of cancer cells. Damaging the DNA essentially damages the manual that instructs the cancer cell to rapidly replicate. Without this manual, the cancer cell either can’t fulfil its duties and dies, or does a poor job at fulfilling its duties, slowing down its rate of replication.
Not only is the CyberKnife an ideal treatment option for dogs with tumors that cannot be reached with surgery, but it also greatly reduces the timeline of treatment overall because of the high dose of radiation it can provide.
For example, a nasal tumor in a dog may take 15 to 20 fractions with conventional radiation, but would only take 3 fractions using the CyberKnife.1 This more limited timeline means less anesthesia, fewer trips to the veterinary office, less stress for your dog, and fewer side effects from the treatment itself.
The CyberKnife can also be used as a supportive tool that works in conjunction with other treatment methods. There is evidence to show that it works well for dogs with cancer when used in tandem with chemotherapy, for example.5
Cancers CyberKnife Can Treat
CyberKnife is typically used for cancers that develop or spread in areas that cannot be operated on, such as the brain. It may also be used for cancers that are very complex in nature, and therefore not suitable candidates for surgery.
Tumors found in the head appear to be the most commonly treated with the CyberKnife. Out of 230 tumor cases treated with the CyberKnife at the Animal Specialty Center in Yonkers, New York, about 50% were brain cancer, 41% were nasal/sinus cavity cancer, and 19% were bone cancer. There is also evidence to suggest that CyberKnife is overall more effective than conventional radiation when it comes to brain cancer in dogs specifically.2
How to Get the Best Results from CyberKnife
The number of CyberKnife treatments is much lower than with conventional radiation, but they are done in quicker succession. A dog receiving three fractions may receive them over the course of three straight days. Be ready to commit a larger chunk of time to finish the radiation treatment plan as scheduled so that it is most effective.
Because your dog will be put under anesthesia, you may also want to consider the following in preparation for the procedure:
- Do not feed your dog the night before radiation.
- Do not provide water to your dog starting a few hours before the procedure.
- Tell your veterinarian about the prescribed and over-the-counter medications that your dog is on, as well as any supplements, as these may need to be stopped prior to receiving anesthesia.
Home Care After CyberKnife Treatments
Aftercare is fairly minimal for CyberKnife irradiation because the procedure is noninvasive. There is no hole, like there would be in a surgery, for example. However, your dog may feel weak, drowsy, or nauseous from the anesthesia. This can last anywhere from 12 to 48 hours post-procedure.
You should aim to keep your dog safe and comfortable after any procedure involving anesthesia. This includes:
- Setting up a quiet and comfortable space for rest.
- Keeping your dog indoors except to go to the bathroom (potty pads may be a good idea if your dog will use them).
- Keeping your dog away from stairs.
- Providing access to water and a small amount of food.
Follow Up Treatments and Tests
Follow up treatments, tests, and care will be based on your dog’s individual clinical signs. These follow ups will likely continue months to years into the future to ensure that no delayed adverse effects have occurred as a result of the radiation treatment.
Your dog may not require any follow up treatment at all. Or, your dog may need:
- Corticosteroid administration if demyelination (loss of the protective covering that surrounds nerve fibers) occurs.
- Antiepileptic administration to prevent seizures or convulsions, which may occur due to abnormal electrical activity in the brain.
- Antiemetic administration to prevent nausea and vomiting.
- Repeat imaging with MRI or a CT scan to reassess the tumor.
When to Not Use CyberKnife
The CyberKnife is not the ideal option for every type of tumor. Keep in mind that although CyberKnife has some incredible benefits and applications, other treatment options may still be preferred.
For example, surgery is typically the best option for mast cell tumors, and surgery is the only option for soft tissue sarcomas.
Ultimately, your dog’s age, tumor type, tumor location, stage of disease, and your family’s goals will dictate if radiation using the CyberKnife is a viable option.
CyberKnife treatments are also lengthy, and your dog will be under anesthesia longer for each fraction than if she undergoes traditional radiation or stereotactic radiation (SRT).
CyberKnife may not be appropriate for dogs who are at an increased risk for anesthetic complications.
Where to Get CyberKnife Treatments
The CyberKnife is only available at a few specialty facilities. In 2014, the CyberKnife was only in clinical use at two veterinary referral centers in the United States; one in San Diego, California and one in Yonkers, New York.6
It has since expanded and is available at more locations, but you and your dog may still have to travel to get treatment. Many veterinary offices work with partner institutions that have the CyberKnife and may be able to refer you.
Safety and Side Effects to Keep In Mind
Side effects will largely depend on the number of fractions (sessions) your dog needs, and location of the tumor.
Short-term side effects include:
- Temporary inflammation of tissue surrounding the tumor site is common, but usually resolves within two weeks after the completion of treatment.
- More extreme side effects include bone fractures from radiation-induced bone necrosis (death) and tumor regrowth, but this is rare.
The types of tumors treated with CyberKnife are often deep in the body, and cause pain on their own. That’s why generally, any discomfort from radiation is expected to be less than the discomfort experienced from the tumor itself.
Your dog may actually be much more comfortable post-radiation treatment, despite any side effects, because their tumor(s) will hopefully be smaller in size.
There are some delayed adverse effects that may occur months, or even years, after radiation is complete:
- Fibrosis (thickening and scarring of bodily tissue)
- Alopecia (hair loss)
- Hypopigmentation (skin discoloration)
- Necrosis (death of bodily tissue)
While you certainly want to keep these in mind, it may not be likely that your dog will experience these side effects. One study found that less than 5% of humans suffered any severe side effects post-radiation treatment five years later.4
Costs Associated with CyberKnife
Radiation treatment with the CyberKnife is expensive. Cost is dependent on multiple factors, including the location of the tumor, the type of tumor, and the number of fractions needed.
The cost of SRT, which the CyberKnife accomplishes, can range anywhere from $2,000 to $9,000. In 2014 the cost of imaging, treatment, and anesthesia for treatment with a CyberKnife was between $7,500 to $8,000.9
Dr. Ettinger explains how Cyberknife works and in which cancers it might be used in this episode of DOG CANCER ANSWERS.
Radiation technician Jenny Fisher explains all about radiation in this must-listen episode of DOG CANCER ANSWERS.
- Bloomfield, R. 2015. Stereotactic radiation therapy in veterinary medicine. Canadian Veterinary Journal 56:95-97. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4266068/.
- Carter, G.L., Ogilvie, G.K., Mohammadian, L.A., Bergman, P.J., Lee, R.P, Proulx, D.R. 2021. CyberKnife sterotactic radiotherapy for treatment of primary intracranial tumors in dogs. Journal of Veterinary Internal Medicine 34:1480-1486. https://onlinelibrary.wiley.com/doi/full/10.1111/jvim.16086.
- CyberKnife. 2022. CyberKnife – How it Works. Available at: https://cyberknife.com/cyberknife-how-it-works/. Accessed on November 4, 2022.
- Emami, B., Lyman, J., Brown, A., Coia, L., Goitein, M., Munzenrider, J.E., Shank, B., Solin, L.J., Wesson, M. 1991. Tolerance of normal tissue to therapeutic radiation. International Journal of Radiation Oncology, Biology, Physics 15:109-122. https://pubmed.ncbi.nlm.nih.gov/2032882/
- Moirano, S.J., Dewey, C.W., Haney, S., Yang, J. 2020. Efficacy of frameless stereotactic radiotherapy for the treatment of presumptive canine intracrainial gliomas: A retrospective analysis (2014-2017). Veterinary and Comparative Oncology 18:528-537.
- Rossmeisl, J.H. 2014. New treatment modalities for brain tumors in dogs and cats. Veterinary Clinics of North America: Small Animal Practice. 44:1013-1038.
- Veterinary Radiation Oncology Treatments for Pets. BluePearl. https://bluepearlvet.com/hospital/bluepearl-veterinary-cyberknife-cancer-center/specialties-services/#:~:text=CyberKnife%20treatment%20for%20pets%20is,to%20an%20almost%20unrecognizable%20level. Published April 21, 2022. Accessed December 9, 2022.
- Radiation Oncology. VCA California Veterinary Specialists. https://vcahospitals.com/california-veterinary-specialists-murrieta/departments/radiation-oncology. Accessed December 9, 2022.
- Stereotactic Radiation Therapy in Dogs. Conditions Treated, Procedure, Efficacy, Recovery, Cost, Considerations, Prevention. https://wagwalking.com/treatment/stereotactic-radiation-therapy. Published September 30, 2021. Accessed December 9, 2022.
- Boatright K. Preparing your dog for anesthesia: Everything owners should know. Pawlicy Advisor. https://www.pawlicy.com/blog/dog-anesthesia/#before. Published January 3, 2022. Accessed December 9, 2022.
CyberKnife® is a trademark of Accuray Incorporated
Topics
Did You Find This Helpful? Share It with Your Pack!
Use the buttons to share what you learned on social media, download a PDF, print this out, or email it to your veterinarian.